How I Took Control of My Health: A Real Talk Guide to Managing Weight with Chronic Conditions
Living with a chronic condition while trying to manage weight can feel like walking uphill in the dark. I’ve been there—frustrated, confused, and tired of quick fixes that don’t last. It’s not just about looking better; it’s about feeling stronger, having more energy, and taking real control. This journey isn’t about perfection. It’s about small, sustainable changes that actually work when health gets complicated. Let me walk you through what truly helped.
Understanding the Weight-Chronic Illness Cycle
When a chronic illness becomes part of daily life, weight often becomes an unintended side effect. Conditions such as type 2 diabetes, hypothyroidism, polycystic ovary syndrome (PCOS), and rheumatoid arthritis can directly influence metabolism, appetite regulation, and energy levels. These are not just labels on a medical chart—they represent real shifts in how the body functions. For instance, insulin resistance in diabetes can promote fat storage, especially around the abdomen, while underactive thyroid function slows down calorie burning, making weight gain easier and weight loss harder, even with strict eating habits.
The relationship between chronic illness and weight is not one-sided. Excess weight, in turn, can worsen disease symptoms. Carrying extra pounds increases stress on inflamed joints in arthritis, raises blood pressure in heart conditions, and deepens insulin resistance in metabolic disorders. This creates a cycle—illness contributes to weight gain, and weight gain intensifies the illness. Recognizing this loop is the first step toward breaking it. The key is understanding that the struggle is not a personal failure. It’s a physiological reality shaped by hormones, inflammation, and medication effects.
Medications commonly prescribed for chronic conditions often add another layer of complexity. Corticosteroids used in autoimmune diseases can increase appetite and promote fluid retention. Some antidepressants and beta-blockers are associated with modest weight gain over time. These side effects are well-documented and not a reflection of willpower. Similarly, chronic inflammation—a hallmark of many long-term illnesses—can interfere with leptin and ghrelin, the hormones that regulate hunger and fullness. When these signals are disrupted, the body may continue to crave food even when energy needs are met.
It’s important to acknowledge that fatigue, pain, and brain fog—common symptoms of chronic conditions—also reduce the capacity for physical activity and mindful eating. A person dealing with fibromyalgia may find it difficult to stand in the kitchen for long periods, limiting meal preparation. Someone with chronic fatigue syndrome may lack the energy to cook altogether, leading to reliance on processed convenience foods. These practical barriers are often overlooked in mainstream weight advice, which tends to focus on motivation rather than medical reality. The truth is, managing weight with a chronic illness requires a different approach—one that respects the body’s limits while supporting its healing.
Why Traditional Diets Fail with Chronic Conditions
Most popular diets are designed for healthy individuals with consistent energy levels and no metabolic complications. They emphasize calorie deficits, rigid meal plans, and high-intensity workouts—strategies that can backfire when applied to someone managing a chronic illness. Severe calorie restriction, for example, may lead to short-term weight loss but often triggers metabolic slowdown, especially in those with thyroid issues or long-term dieting history. The body interprets low intake as a threat and conserves energy, making future weight loss more difficult and regain more likely.
Another common pitfall is the expectation of rapid results. Many women in their 30s to 50s report feeling defeated when they follow a trendy diet—keto, intermittent fasting, or juice cleanses—only to see minimal change on the scale. This can lead to frustration, shame, and a sense of personal failure, even though the real issue may be hormonal imbalance or medication effects. Diets that eliminate entire food groups may also deprive the body of essential nutrients needed for immune function, hormone production, and tissue repair—critical needs for anyone with a chronic condition.
Exercise recommendations in mainstream programs often assume a level of physical ability that many with chronic illness do not have. Being told to “just walk 10,000 steps” or “do 30 minutes of cardio” can feel dismissive when joint pain, fatigue, or dizziness limits mobility. Pushing too hard can lead to flare-ups, injury, or post-exertional malaise, particularly in conditions like lupus or chronic fatigue syndrome. The result is a pattern of starting strong, overdoing it, crashing, and giving up—only to repeat the cycle months later.
What’s needed instead is flexibility and personalization. A sustainable approach acknowledges that energy levels fluctuate and that some days will be better than others. It replaces rigid rules with adaptable habits—such as eating balanced meals when possible, moving gently when able, and resting without guilt. Success is measured not by the speed of weight loss but by improved energy, better sleep, and reduced symptoms. This mindset shift—from restriction to support—is what makes long-term progress possible.
Building a Health-First Mindset (Not Just Weight Loss)
Shifting the focus from weight loss to overall health is a powerful step in managing chronic conditions. For many women, the scale has been a source of anxiety for years, dictating self-worth and daily mood. But when health is compromised, the number on the scale becomes a less reliable indicator of progress. A more meaningful measure includes how you feel—whether you can play with your grandchildren without shortness of breath, stand in the kitchen long enough to cook a meal, or wake up with less joint stiffness.
Progress can also be seen in lab results: lower HbA1c levels in diabetes, improved cholesterol panels, or reduced inflammatory markers like CRP. These are tangible signs that the body is responding to positive changes, even if the scale doesn’t move. Tracking non-scale victories—such as needing less medication, sleeping more soundly, or feeling more alert during the day—helps build confidence and motivation. It shifts the narrative from “I haven’t lost enough weight” to “I am taking care of my body in ways that matter.”
Self-compassion is a cornerstone of this mindset. It means treating yourself with the same kindness you would offer a close friend facing similar challenges. It means recognizing that setbacks are part of the process, not proof of failure. On days when fatigue wins and the workout doesn’t happen, self-compassion allows you to rest without guilt. On days when comfort food is chosen over a “perfect” meal, it allows you to eat without shame. This non-judgmental awareness reduces stress, which in turn supports better hormonal balance and emotional regulation.
Mental resilience plays a crucial role in long-term health. Chronic illness often brings a sense of loss—of the body you once had, the activities you once enjoyed, or the future you imagined. Accepting this reality without giving up is an act of courage. It involves making peace with limitations while still striving for improvement. This balanced perspective fosters patience and persistence. It helps you stay committed to small, daily actions that add up over time. When the goal is not a number but a better quality of life, the journey becomes more sustainable and more meaningful.
Food That Works With Your Body, Not Against It
Nutrition is a powerful tool for managing chronic conditions and supporting healthy weight. The goal is not extreme dieting but consistent, balanced eating that stabilizes blood sugar, reduces inflammation, and sustains energy. Meals should include a combination of protein, fiber-rich carbohydrates, and healthy fats. This trio slows digestion, prevents blood sugar spikes, and promotes satiety. For example, a breakfast of Greek yogurt with berries and a sprinkle of chia seeds provides protein, antioxidants, and omega-3s—supporting metabolic and immune health.
Simple food swaps can make a big difference. Choosing whole grains like quinoa or oats over refined white bread helps maintain steady energy and supports gut health. Replacing sugary snacks with nuts, fruit, or hummus with vegetables reduces insulin demand and inflammation. Cooking at home more often allows better control over ingredients, reducing intake of hidden sugars, unhealthy fats, and excess sodium found in processed foods. These changes don’t require perfection—just a gradual shift toward more whole, nutrient-dense foods.
Hydration is another key factor. Dehydration can mimic hunger and contribute to fatigue and constipation—common issues in chronic illness. Drinking water throughout the day, especially before meals, can support digestion and appetite regulation. Herbal teas like ginger or peppermint may also soothe digestion and reduce bloating. Limiting sugary drinks, including fruit juices and sweetened coffee, helps prevent blood sugar swings and unnecessary calorie intake.
Mindful eating—paying attention to hunger and fullness cues—can improve digestion and prevent overeating. This means eating without distractions, chewing slowly, and checking in with your body during meals. For those with limited energy, preparing meals in batches or using slow cookers can reduce daily effort while ensuring access to healthy options. The focus is on consistency, not intensity. Eating well most of the time, even if not perfectly, creates a foundation for long-term health.
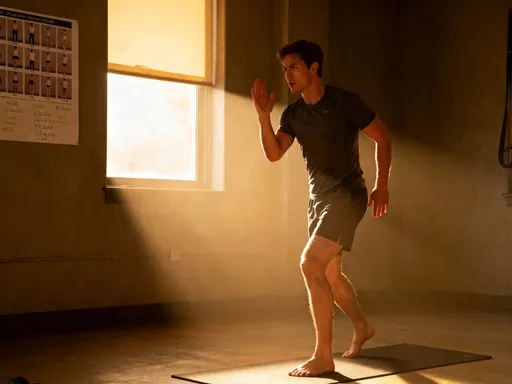
Movement That Fits Your Energy, Not Drains It
Physical activity is essential, but for those with chronic conditions, the type and intensity must be carefully matched to energy levels and physical capacity. The goal is not to burn calories but to support circulation, joint mobility, mood, and metabolic function. Movement should feel like a gift to the body, not a punishment. Even small amounts, when done regularly, can yield significant benefits.
Low-impact activities are often the most sustainable. Walking, especially in nature, combines gentle exercise with stress reduction. Water aerobics or swimming reduce joint strain while building strength and endurance. Chair yoga or seated stretching routines can improve flexibility and circulation for those with limited mobility. These activities can be done in short sessions—10 to 15 minutes at a time—and gradually increased as tolerance improves.
Listening to the body is crucial. Some days may allow for longer walks or more active movement; other days may call for rest or gentle stretching. Honoring these fluctuations prevents burnout and injury. Using tools like a pedometer or fitness tracker can help monitor activity without pressure—focusing on progress, not perfection. The aim is to move more than you did yesterday, not to meet arbitrary goals.
Strength training, even with light resistance bands or body weight, helps preserve muscle mass, which naturally declines with age and inactivity. Muscle tissue burns more calories at rest than fat, so maintaining it supports metabolic health. Balance exercises, such as standing on one foot or heel-to-toe walking, reduce fall risk and improve coordination. These elements can be incorporated into daily routines—while brushing teeth or waiting for the kettle to boil—making movement accessible and manageable.
Sleep, Stress, and the Hidden Triggers
Sleep and stress are often overlooked but deeply connected to weight and chronic illness. Poor sleep disrupts hormones that regulate hunger—increasing ghrelin (the hunger hormone) and decreasing leptin (the fullness hormone). This can lead to increased appetite, especially for high-carb, high-fat foods. For women managing conditions like fibromyalgia or hypertension, poor sleep can also worsen pain and elevate blood pressure, creating a cycle that’s hard to break.
Chronic stress activates the sympathetic nervous system, leading to elevated cortisol levels. Over time, high cortisol promotes fat storage, particularly around the abdomen, and increases insulin resistance. It can also trigger emotional eating and reduce motivation for healthy habits. Managing stress is not a luxury—it’s a medical necessity for those with long-term health conditions.
Science-backed strategies can help. Establishing a wind-down routine—an hour before bed without screens, using dim lighting, and engaging in calming activities like reading or light stretching—signals the body that it’s time to rest. Breathwork techniques, such as diaphragmatic breathing or box breathing, can calm the nervous system in minutes. Spending time in nature, even a short walk in a park, has been shown to lower cortisol and improve mood.
Digital detoxing—reducing screen time, especially in the evening—can improve sleep quality and reduce mental fatigue. Setting boundaries around work, caregiving, or household demands is also important. Learning to say no, asking for help, and scheduling rest are acts of self-care that support long-term health. When sleep improves and stress is managed, the body has a better chance to heal, regulate hormones, and maintain a healthy weight.
Putting It All Together: Small Steps, Big Impact
Integrating these changes doesn’t require a complete lifestyle overhaul. A realistic approach starts with one small habit at a time. For example, begin by adding a serving of vegetables to one meal daily, or take a five-minute walk after dinner. Once that feels routine, build on it—add another walk, swap a sugary snack, or try a new relaxation technique. The key is consistency, not speed.
Tracking progress can be helpful, but the focus should be on how you feel, not just numbers. Keeping a simple journal to note energy levels, mood, sleep quality, and symptoms can reveal patterns and reinforce motivation. Celebrating small wins—like choosing water over soda, or resting when tired—builds confidence and reinforces positive behavior.
It’s important to remember that progress is not linear. There will be days when symptoms flare, energy dips, or old habits return. These are not failures but part of the journey. What matters is returning to your intentions with kindness and without self-criticism. Each choice to nourish, move, rest, or seek support is a step toward greater well-being.
Working with healthcare providers—doctors, dietitians, physical therapists—is essential for creating a safe, personalized plan. They can help adjust medications, monitor lab work, and recommend appropriate exercises or dietary changes based on your specific condition. This collaboration ensures that your efforts are supported by medical expertise and tailored to your needs.
Conclusion: Your Health, Your Power
Managing weight with a chronic illness is not about willpower or quick fixes. It’s about making sustainable, compassionate choices that honor your body’s needs. It’s about shifting focus from appearance to vitality, from restriction to nourishment, from isolation to support. Every small decision—to eat a balanced meal, to rest when tired, to move gently—adds up to a life of greater strength and freedom.
You are not alone in this journey. Millions of women navigate similar challenges every day, finding ways to thrive despite health complications. The courage to keep trying, to show up for yourself even on hard days, is what defines true health. With the right mindset, practical strategies, and professional support, sustainable change is possible. Your health is not defined by your diagnosis—it is shaped by the choices you make, one day at a time. And every choice matters.